In those with underlying medical issues such as diabetes, obesity, or high blood pressure, COVID-19 is a respiratory infection that can lead to severe sickness. To determine if one is currently infected with SARS-CoV-2, the coronavirus that causes COVID-19, there are often two different tests done.
A polymerase chain reaction (PCR) test, often known as a diagnostic or molecular test, is the first kind. By detecting the coronavirus’ genetic material, a PCR test can aid in diagnosing COVID-19. The CDC is short for the Centers for Disease Control and Prevention. Regards PCR tests as the gold standard for diagnosis. An antigen test is the second type by looking for specific chemicals on the surface of the SARS-CoV-2 virus; these assays aid in diagnosing COVID-19. Learn more the signs that may show that one needs a rapid antigen test.
The term “rapid tests” refers to COVID-19 tests that don’t need to be run via a lab and can produce findings in as little as 15 minutes. Typically, they come in the form of antigen testing. Rapid tests can yield findings quickly but lack the same precision level as PCR tests examined in a laboratory. Read on by reading on, learn about quick tests’ accuracy and when to use them in place of PCR tests.
How reliable are rapid antigen tests?
Rapid COVID-19 testing frequently yields answers in just a few minutes and doesn’t require specialized laboratory analysis.
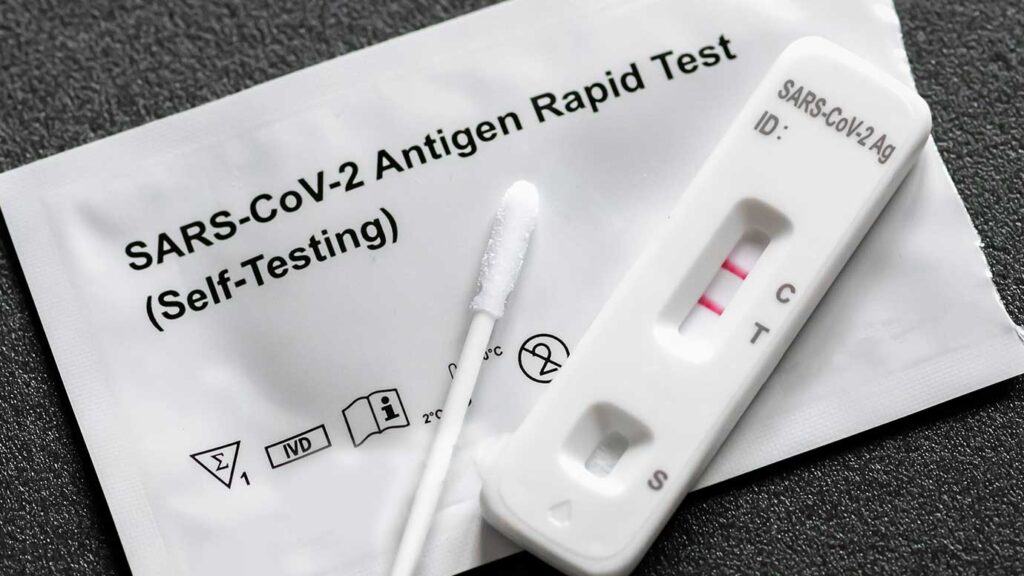
Most rapid tests are antigen tests, using the two terms simultaneously. However, since the FDA has also approved laboratory-based antigen tests, the CDC has stopped referring to them as “rapid” tests.
- Rapid antigen tests, often known as point-of-care exams, can be carried out at:
- a house and a home, a pharmacy, a doctor’s office, a school clinic, and COVID-19 tests
- airports, long-term care homes, and drive-through testing locations
To collect mucus and cells for the test, you or a medical practitioner will insert a cotton swab into your nose, throat, or both. The sample is often placed on a strip that changes colour if you test positive for COVID-19.
Although these tests yield findings quickly, they are less reliable than laboratory tests since a positive test requires a higher virus concentration in your sample. Rapid testing provides a significant risk of returning a false negative. If the test results indicate that you do not have COVID-19 when you do, this is a false negative.
How reliable are tests done at home?
Although at-home testing isn’t as precise as gold standard PCR tests, they still help identify COVID-19 cases that might not have been discovered otherwise. Home COVID-19 testing, like other antigen COVID-19 tests, has a more significant possibility of a false negative than a false positive, which means it’s more likely to say you have COVID-19 when you don’t do.
To identify COVID-19 infection, researchers compared the accuracy of at-home antigen tests to PCR lab tests. The home tests accurately identified 78.9% of persons who did have the virus and correctly identified 97.1% of people who did not have the virus during days 0 to 12 after symptoms start.
Home tests correctly detected 96.2 of COVID-19 patients when administered within three days of symptom onset. The researchers discovered tests performed three days after the start of symptoms were nearly as accurate as those performed on the first day of symptoms.
Why is Rapid antigen test preferred
Rapid COVID-19 testing has various advantages over PCR tests despite having a relatively significant risk of false negative results. Rapid antigen tests can deliver findings in seconds rather than days; they are more portable and available than lab tests, are less expensive than lab tests, and don’t call for an expert or lab.
Rapid COVID-19 testing is available in many crowded places, including airports, arenas, theme parks, and other areas with high pedestrian traffic. While rapid tests won’t catch every COVID-19 instance, at least some cases that could have gone undetected could be detected.
What should you do if a quick test comes back negative, but you still have symptoms?
It’s possible that you got a false negative if your quick test indicates that you don’t have the coronavirus but have COVID-19 symptoms.
Confirming your negative result with a more precise PCR test is smart.

How reliable are further COVID-19 tests?
In general, PCR testing is more precise than fast tests. Rarely are CT scans used to identify COVID-19. Tests with antibodies can be used to identify previous infections.
- PCR test
The gold standard for diagnosing COVID-19 is still the PCR covid test. According to a study, 97.2 per cent of the time, mucus PCR tests correctly identified COVID-19.
- CT (Computerized Tomography) scans
Although CT scans aren’t frequently used to diagnose COVID-19, they may be able to do so by detecting lung issues. They are less valuable than other tests, though, and they struggle to rule out other respiratory illnesses.
According to the same study, CT scans accurately detected a positive COVID-19 case 91.9 per cent of the time but only 25.1 per cent of the time a negative COVID-19 case.
- Antibody assays
Antibody testing checks for immune system-produced proteins called antibodies that may indicate a history of coronavirus infection. They specifically search for IgM and IgG antibodies. No, antibody testing. Antibody tests can’t detect the diagnosis of current coronavirus infection.
IgM and IgG antibody testing successfully detected the existence of these antibodies in 84.5 and 91.6 per cent of cases, respectively, according to the January 2021 study.
What to do if you suspect COVID-19
The majority of COVID-19 patients experience mild sickness. You should start isolating yourself from others immediately if you have any reason to believe you have COVID-19. In the absence of a complete coronavirus vaccination or a recent positive COVID-19 result, The CDC continues to advise a 5-day quarantine.
Conclusion
Research indicates quick The first week after symptoms appear when COVID-19 testing is most accurate.
With quick tests, there is a greater danger of receiving a false negative result. Those without symptoms are more likely to receive an incorrect negative impact than those without symptoms. Rapid tests, on the other hand, only provide false positive results about 1% of the time.
An efficient preliminary test to determine whether you have the coronavirus that causes COVID-19 is a quick COVID-19 test. If you experience symptoms even though your fast test is negative, confirming your findings with a PCR test might be a good idea.