Cataracts are a common eye condition that affects millions of people worldwide. As the lens of the eye gradually becomes cloudy, individuals may experience difficulties with vision, impacting their daily activities. Understanding when to undergo cataract surgery can be a daunting task for many. This article aims to provide clarity on cataracts, their symptoms, the process of diagnosis, and deciding the right timing for surgery.
Understanding Cataracts
Cataracts are a clouding of the eye’s natural lens, which is located behind the iris and pupil. This lens is usually clear and helps focus light onto the retina, enabling clear vision. However, as cataracts form, the lens becomes opaque, leading to blurred or distorted vision. The gradual progression of cataracts can often go unnoticed in the early stages, as individuals may adapt to subtle changes in their vision. Over time, however, these changes can become more pronounced, affecting daily activities such as reading, driving, and recognizing faces.
In conclusion, the decision to proceed with eye cataract surgery is profoundly individual and should be based on a combination of symptom severity and personal needs. Regular eye exams and open communication with your eye care provider will ensure you are well-informed about your options and can make timely decisions regarding your eye health.

What are Cataracts?
Cataracts develop gradually, often over several years. They are primarily associated with aging, but they can also occur due to other factors. Although they usually do not cause pain, their progression can significantly affect one’s quality of life. There are various types of cataracts, with age-related cataracts being the most common. Other types include congenital cataracts, which are present at birth, and secondary cataracts that can develop after eye surgery or due to other medical conditions. Understanding the different types of cataracts can help individuals recognize symptoms and seek appropriate treatment.
Causes and Risk Factors of Cataracts
The causes of cataracts can include:
- Aging: As a natural part of the aging process, proteins in the lens begin to break down and clump together, forming cloudy areas.
- Diabetes: Elevated blood sugar levels can lead to changes in the eye’s lens.
- Long-term use of steroids: Certain medications can increase the likelihood of developing cataracts.
- Smoking and Alcohol use: Both habits have been linked to higher risks of cataracts.
- UV Radiation: Prolonged exposure to sunlight can contribute to the development of cataracts.
Both hereditary factors and prior eye injuries can also increase an individual’s risk of cataracts, emphasizing the importance of regular eye examinations. Additionally, certain lifestyle choices, such as maintaining a healthy diet rich in antioxidants and vitamins, may play a role in reducing the risk of cataract formation. Foods high in vitamin C and E, such as citrus fruits, nuts, and leafy greens, can help protect the eyes from oxidative stress, potentially delaying the onset of cataracts. Awareness of these risk factors and proactive health measures can empower individuals to take charge of their eye health.
Learn about cataracts treatments at: What Are the Latest Advances in Cataracts Treatment
Symptoms of Cataracts
The symptoms of cataracts may not be immediately noticeable. However, as the condition progresses, individuals may find their vision affected significantly.

Early Stage Symptoms
In the early stages, one may experience mild symptoms such as:
- Blurred or cloudy vision
- Difficulty seeing in low light conditions
- Increased sensitivity to glare
- Seeing halos around lights
- Frequent changes in prescription glasses or contact lenses
These symptoms might initially be manageable, but over time can worsen, prompting further vision disturbances. Many individuals may not realize that these changes in vision are related to cataracts, attributing them instead to normal aging or fatigue. Regular eye examinations become crucial during this stage, as an eye care professional can provide a comprehensive assessment and monitor any changes in vision. Early detection can lead to better management strategies, including lifestyle adjustments such as improved lighting for reading or using anti-glare lenses. Learn more about fatigue on https://www.health.harvard.edu/staying-healthy/fighting-fatigue
Advanced Stage Symptoms
As cataracts progress to more advanced stages, symptoms become more pronounced. They may include:
- Significant loss of vision in one or both eyes
- Difficulty reading or performing tasks that require clear vision
- Yellowing or fading of colors
- Persistent double vision
At this stage, individuals may need to consider surgical options to restore their vision and improve their quality of life. The decision to undergo surgery often stems from the impact cataracts have on daily activities, such as driving, working, or enjoying hobbies. Moreover, many patients report a profound emotional response to their vision changes, as the gradual loss can lead to feelings of frustration and isolation. Understanding the surgical process, including the types of cataract surgery available, can empower individuals to make informed choices about their eye health and regain their independence.
The Process of Diagnosing Cataracts
Diagnosis of cataracts typically involves a comprehensive eye examination performed by an eye care professional. This examination is essential for determining the extent of vision impairment and crafting a suitable treatment plan. Early detection is crucial, as timely intervention can significantly improve quality of life and prevent further deterioration of vision.
Eye Examination
An eye examination includes a variety of tests. The eye doctor will check your vision and look for signs of cataracts by using specialized equipment to examine the lens and retina. They assess the clarity of the lens and monitor cloudiness, helping to establish the severity of the cataracts. In addition to visual assessments, the doctor may also perform a slit-lamp examination, which allows for a detailed view of the eye’s structures, including the cornea, iris, and lens. This thorough evaluation helps in identifying any other underlying eye conditions that may be present alongside cataracts.
Visual Acuity Test
During a visual acuity test, the eye care professional utilizes an eye chart to measure how well you see at different distances. This test helps to quantify the impact of cataracts on your vision and provides a clearer picture of whether surgical intervention is necessary. The results of this test are often compared to previous examinations to track changes over time, which can be particularly useful in monitoring the progression of cataracts. Furthermore, the eye doctor may also assess your contrast sensitivity, which evaluates your ability to distinguish between different shades of light and dark. This aspect of vision can be significantly affected by cataracts, and understanding it can help in making informed decisions regarding treatment options. To read more about sensitivity click here.
Deciding on the Right Time for Surgery
When considering cataract surgery, it is essential to evaluate various factors that could influence the decision.
Evaluating Your Symptoms
Assessing the severity of your symptoms is critical. If everyday tasks such as reading, driving, or working at a computer have become increasingly difficult, it might indicate that surgery is warranted. It’s important to openly discuss your symptoms with your eye care provider, as they can provide insight based on your specific situation. Symptoms like blurred vision, halos around lights, or difficulty seeing at night can progressively worsen, making it imperative to monitor these changes closely. Keeping a journal of your visual experiences can help you articulate your concerns more effectively during your consultations.
Considering Your Lifestyle and Needs
Your lifestyle and personal needs play a significant role in the decision to undergo cataract surgery. For instance, if you lead an active lifestyle that requires clear vision, such as driving, traveling, or enjoying outdoor activities, surgical intervention may be a priority. Additionally, many patients opt for surgery when they feel that their quality of life is being impacted. It’s worth noting that some individuals may find that their hobbies, such as reading or crafting, become less enjoyable due to deteriorating vision. In such cases, the emotional and psychological aspects of living with cataracts should not be overlooked, as they can significantly affect overall well-being. Furthermore, discussing the potential outcomes of surgery, including the possibility of improved vision and reduced dependency on glasses, can help clarify your decision-making process.
Preparing for Cataract Surgery
Once you and your eye care provider have determined that surgery is appropriate, preparation becomes key to a successful outcome.
Pre-Surgery Medical Evaluation
A thorough pre-surgery medical evaluation is conducted to ensure you are fit for surgery. This exam will take into account your overall health status, including any medication you may be taking, allergies, and pre-existing health conditions. If you have chronic conditions such as diabetes or heart disease, these will be closely monitored to tailor the surgical approach. Additionally, your eye care provider may perform a series of tests to measure the curvature of your cornea and the size of your eye, which are essential for selecting the right type of intraocular lens (IOL) for your specific needs. Understanding your unique eye anatomy helps in achieving optimal visual outcomes post-surgery.
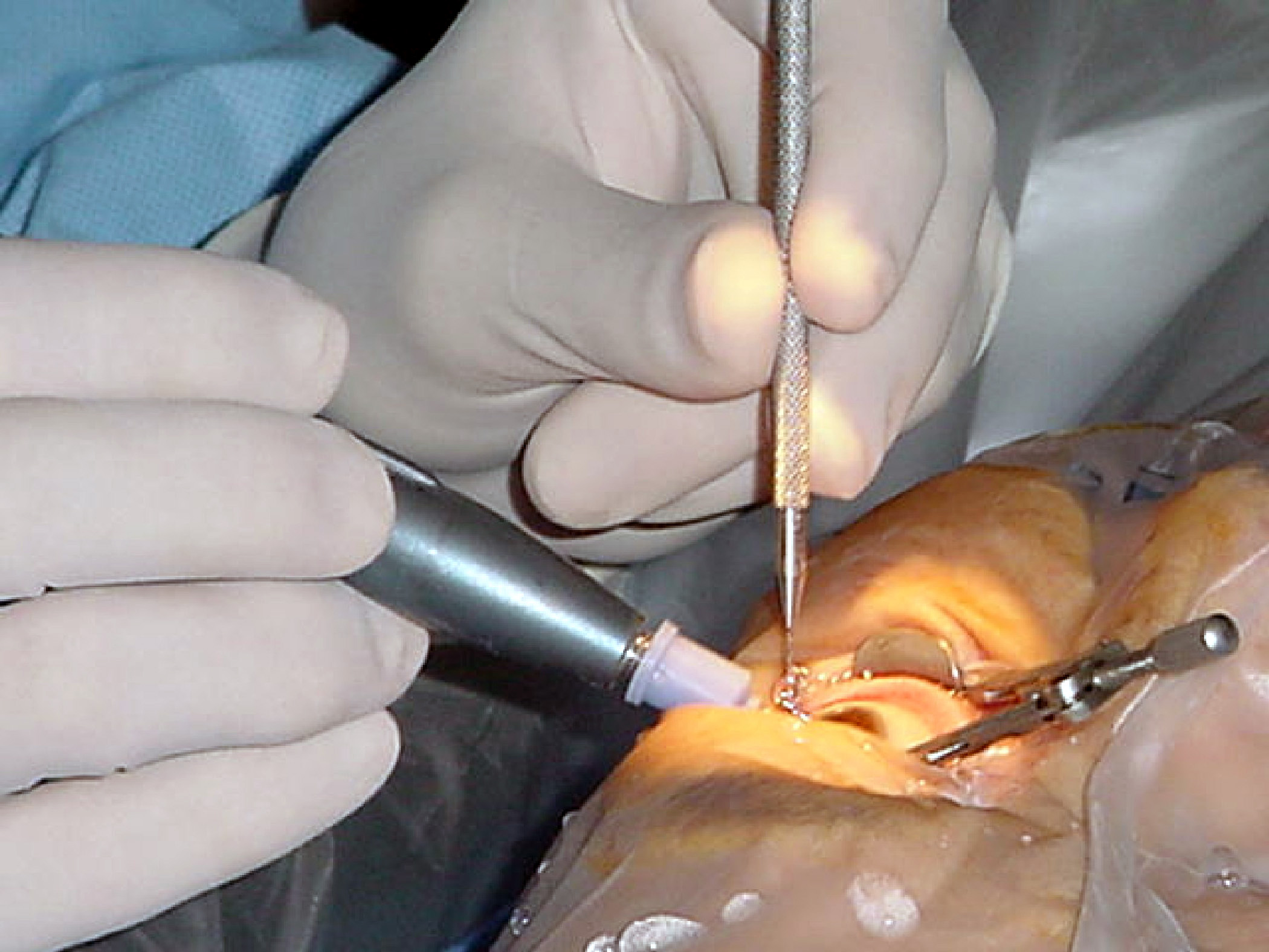
What to Expect on the Day of Surgery
On the day of surgery, patients are typically advised to arrive early. The procedure is usually performed on an outpatient basis, allowing patients to return home on the same day. It generally involves the removal of the cloudy lens and replacement with an artificial intraocular lens. Patients are given local anesthesia to minimize discomfort during the procedure. It’s important to have someone accompany you, as you may feel disoriented after the anesthesia wears off. The surgical team will guide you through the process, explaining each step to alleviate any anxiety you may have.
Post-surgery, individuals may experience some blurred vision or mild discomfort initially, both of which are normal. Follow-up appointments will be crucial to monitor healing and ensure the best visual outcomes. During these visits, your eye care provider will assess your recovery progress and may provide specific instructions regarding eye drops or medications to reduce inflammation and prevent infection. It is also common to be advised to avoid strenuous activities and heavy lifting for a short period after surgery to facilitate healing.